Recently, many anaesthetists were informed about the suspension of surgeries because their patients had been infected with COVID-19.
According to Cai Qingxiang, attending physician at the Department of Anesthesiology of the First Affiliated Hospital of Guangzhou University of Chinese Medicine, the common symptoms of COVID-19 include fever, headache, sore throat, cough, diarrhoea and muscle soreness. Severe cases can develop pneumonia, dyspnea, and respiratory failure.
With the occurrence of hypoxemia brought on by the novel coronavirus infection, many patients may experience pathologic and physiological changes in the respiratory system. Some elderly people may also experience silent hypoxemia. Early-stage imaging reveals numerous small patchy shadows, mostly extrapulmonary, in both lungs.
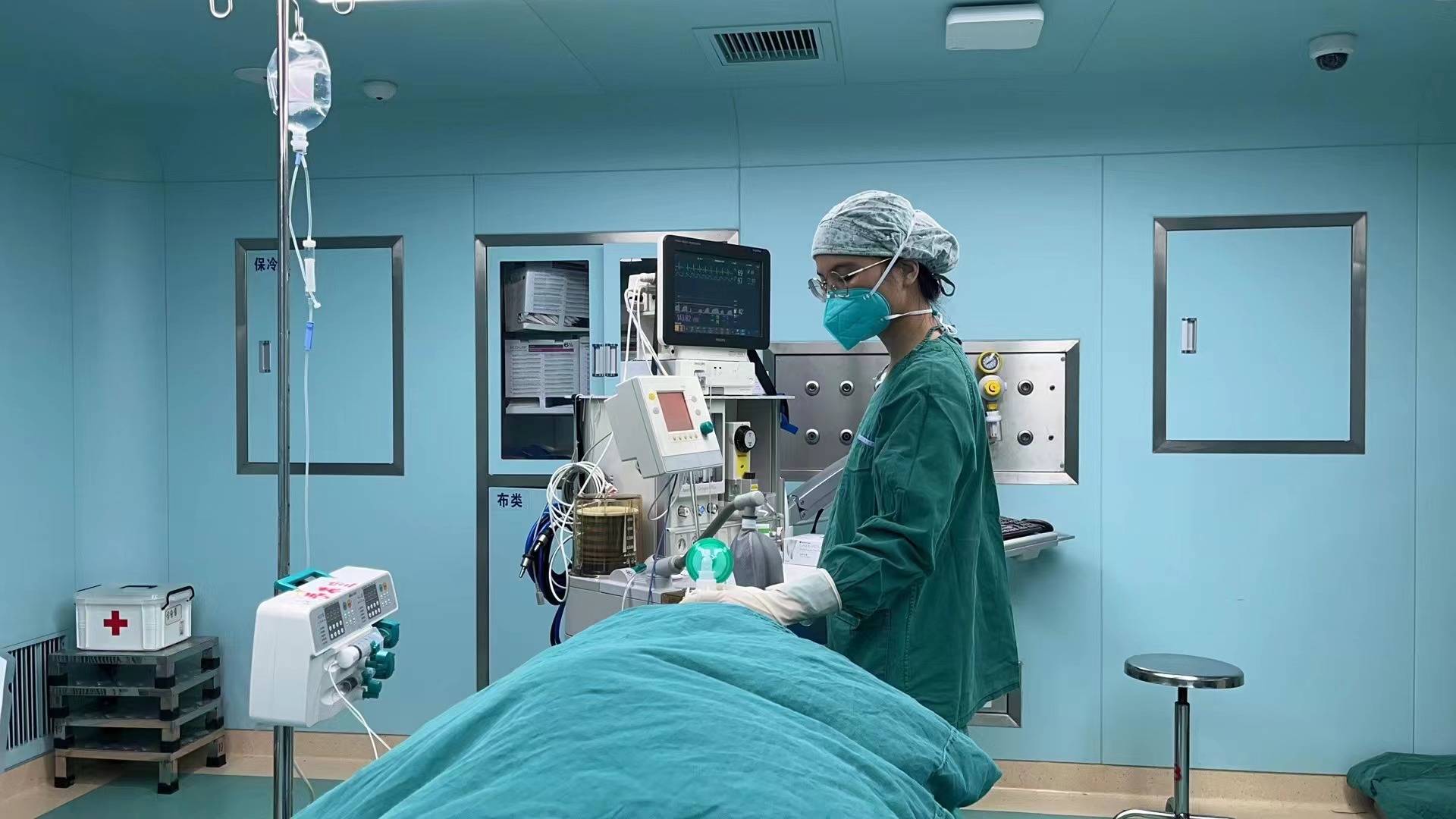
(Photo provided to GDToday)
As the illness progresses, multiple ground-glass opacities and infiltrates in both lungs may appear. In severe cases, pulmonary consolidation may occur, which is often called white lung. At this time, the permeability of the lung tissue is significantly reduced.
The coronavirus invasion may lead to the inflammation of the upper and lower respiratory tracts, and damage the function of the lungs to some extent. Anesthesia may cause the following risks:
1. Airway hyperresponsiveness
2. Insufficient ventilation and hypoxemia
3. Difficult intubation
4. Problems with postoperative rehabilitation
There should be no delay if a medical emergency necessitates surgery, such as a cesarean section or traumatic bleeding, regardless of whether the patients are COVID-19-infected or not.
When patients test positive, they should be cautious about non-emergency surgical procedures, especially individuals with underlying diseases. It's advised to give the body time to recover.
How long can we receive an operation after infection?
It takes a longer time to recover after an infection. Therefore, in the short term, patients will still face greater risks, and it is necessary to treat the severity of the disease differently.
1.Emergency surgery: No matter if you have COVID-19 infection or not, no matter what stage of infection you are in, there is no time to waste when emergency surgery is needed due to the patient's life-threatening condition.
2. Non-emergency surgery: Suspending the surgery in a short time will not threaten the life of the patients. According to the ASA-APSF Joint Statement on Non-Urgent Care During the COVID-19 Outbreak, the suggested wait times from the date of COVID-19 diagnosis to surgery are as follows:
Four weeks for an asymptomatic patient or recovery from only mild, non-respiratory symptoms.
Six weeks for a symptomatic patient (e.g., cough, dyspnea) who did not require hospitalization.
Eight to 10 weeks for a symptomatic patient who is diabetic, immunocompromised, or hospitalized.
Twelve weeks for a patient who was admitted to an intensive care unit due to COVID-19 infection.
It is worth noting that we also need to combine the current patient symptoms, cardiopulmonary recovery, the patient's age, underlying medical conditions, type of surgery, and ASA (American Society of Anesthesiologists) assessment of surgical risk ratings to conduct a comprehensive assessment of operations, so as to further optimize perioperative management.
Author | Hannah, He Yang (intern)
Editor | Wing, Nan, Will, James
















